this post was submitted on 28 Jul 2023
133 points (98.5% liked)
Climate - truthful information about climate, related activism and politics.
5212 readers
667 users here now
Discussion of climate, how it is changing, activism around that, the politics, and the energy systems change we need in order to stabilize things.
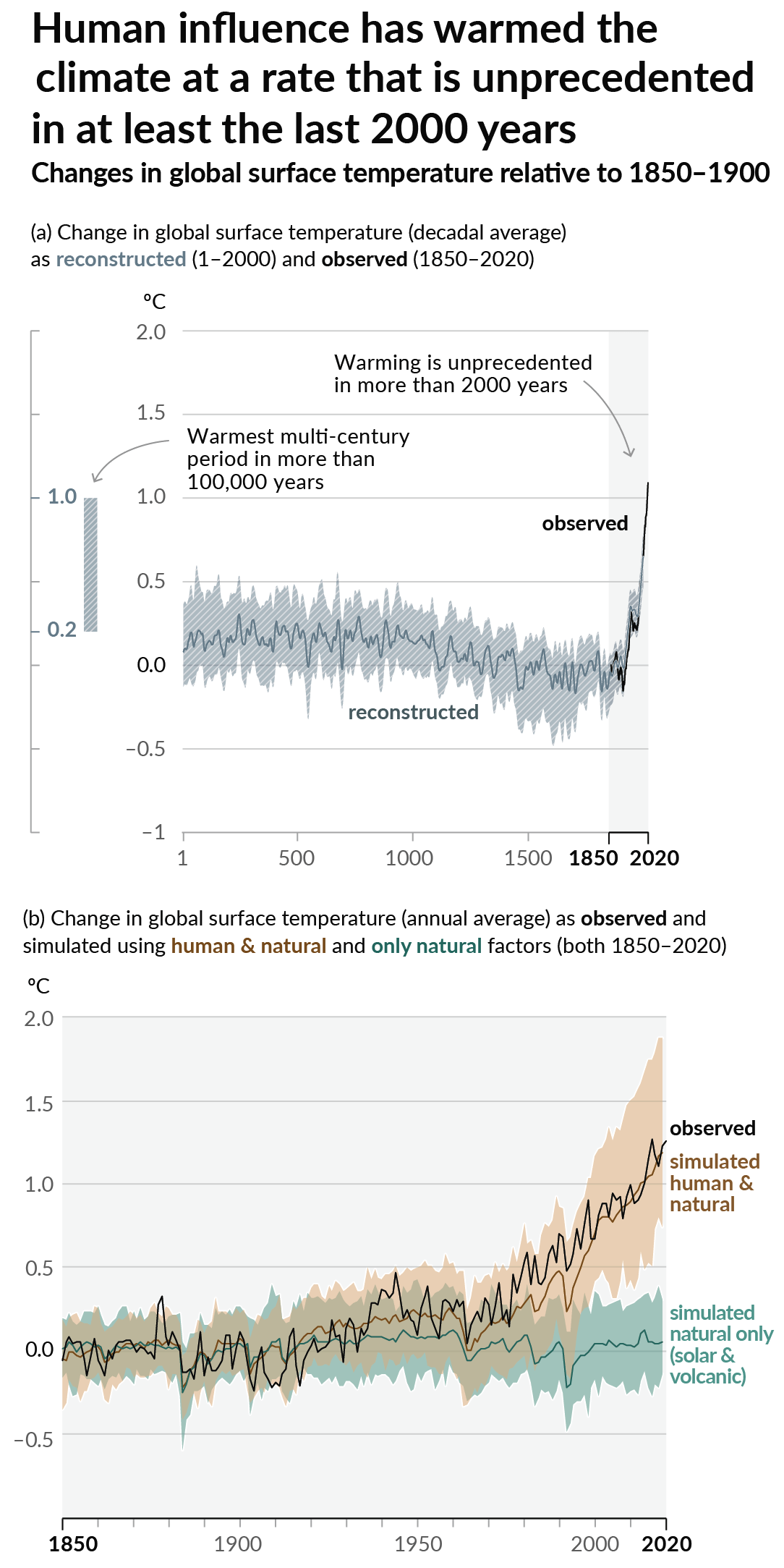
As a starting point, the burning of fossil fuels, and to a lesser extent deforestation and release of methane are responsible for the warming in recent decades:
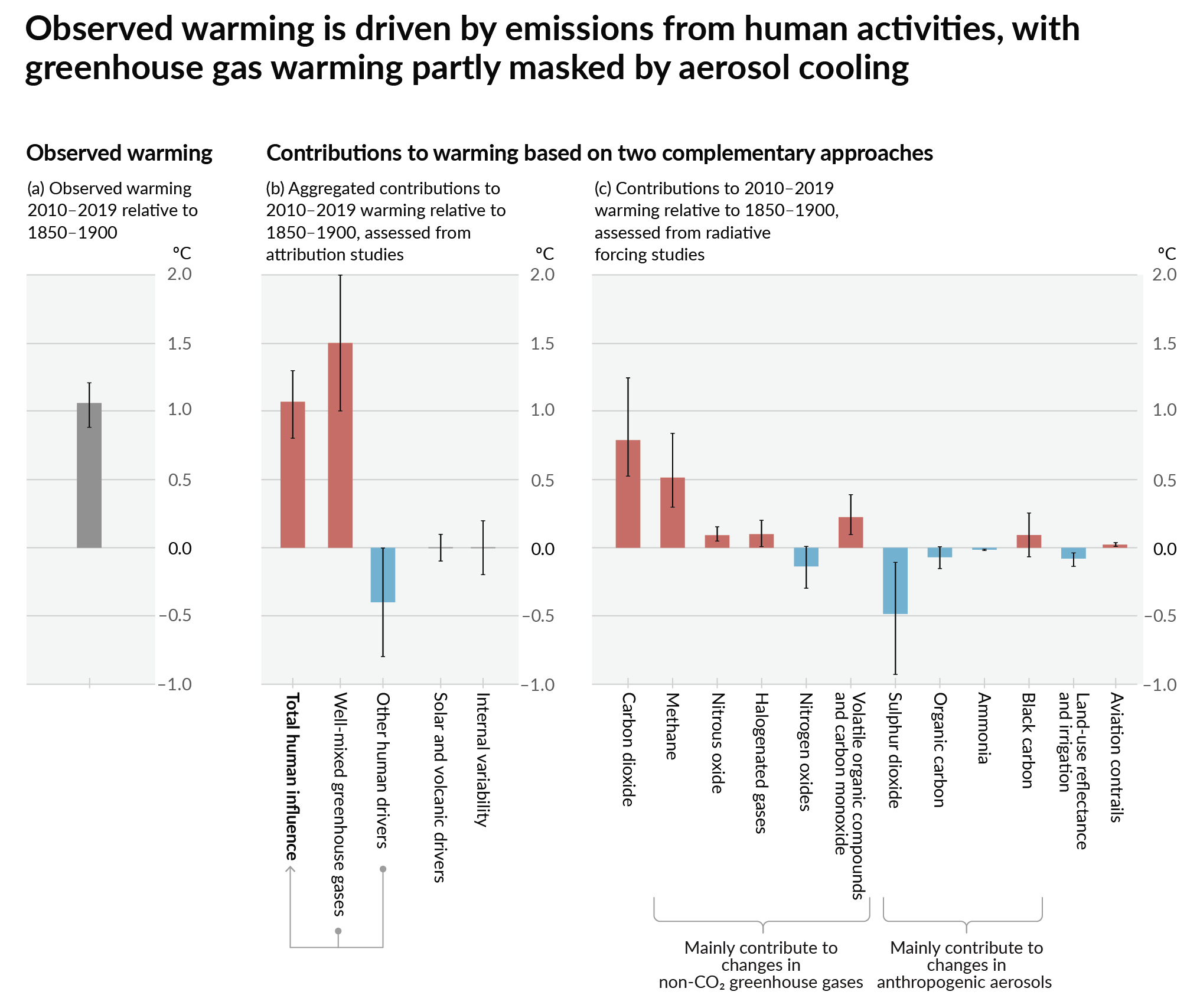
How much each change to the atmosphere has warmed the world:
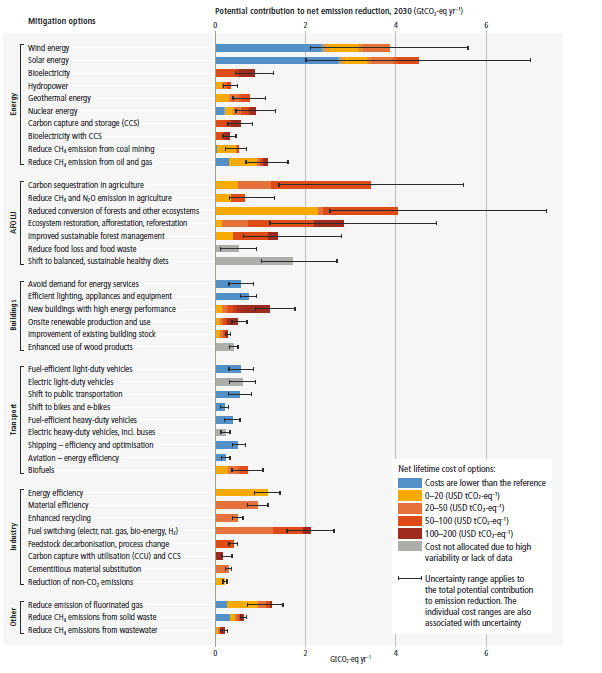
Recommended actions to cut greenhouse gas emissions in the near future:
Anti-science, inactivism, and unsupported conspiracy theories are not ok here.
founded 1 year ago
MODERATORS
you are viewing a single comment's thread
view the rest of the comments
view the rest of the comments
That's the rate when an infection establishes itself in blood. In a known outbreak (Royal Brompton Hospital), I recall that 9 patients out of 50 (18%) developed candidemia, but none of them died.
However, a study from India reports:
Notes:
C. auris is observed together with other pathogens like C. rugosa and C. tropicalis, leading to the question of which of them is the killer, or whether co-infection is the killer
the mortality rate is given as a percent of people who developed candidemia (had Candida infections in their bloodstream), not as a percent of the total; upon hasty reading this can fool a person, and has fooled people before
the mortality rate is split into two variables: crude mortality (the patient is dead, the patient tests positive) and attributable mortality (the patient is dead, we can see how Candida killed the patient)
they found correlations which increased the risk; since they list "admission to a public sector hospital" among the factors, low standards of care in the Indian public healthcare system, or lack of experience in dealing with Candida (including wrong treatment protocols) may explain part of excess mortality
The study from Venezuela (a country afflicted with civil conflict and poverty) reports:
Unfortunately, the summary does not give adequate clues to understand the underlying conditions of the people (as I notice - mostly children). It mentions they were "critically ill", but doesn't mention if they were critically ill with Candida or before getting Candida. With such statistics as given in the summary - it is truly hard to evaluate the danger posed by a pathogen, because it's hard to isolate it from other factors. However, 30-day mortality was 28%, which is miserable.
My main conclusion seems to be: the first line of defense is having a hospital system that is ready to detect and deal with Candida. If this exists, many deaths can be avoided.
Of course, vaccination would be far preferable to combating it at a later stage.